Dentoalveolar Surgeries
Expert surgical management of teeth and supporting structures
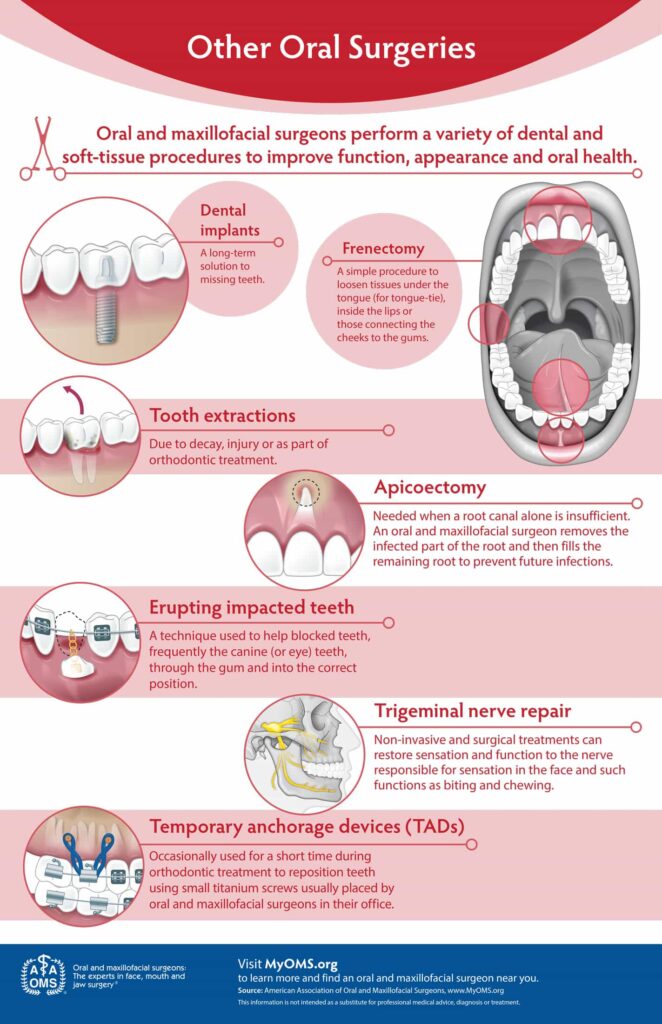
The surgical management of soft and hard tissues is at the core of what oral and maxillofacial surgeons are trained to do. Dentoalveolar surgeries involve the alveolar bone and supporting structures, including:
1. Removal of Impacted Teeth
Purpose: Extract teeth that are trapped in the jawbone or gums, often causing pain, infection, or crowding.
Common Cases:
- Third molars (wisdom teeth)
- Impacted canines or premolars
Techniques:
- Simple extraction (for erupted teeth)
- Surgical extraction (for impacted/bony impactions)
- Piezoelectric surgery (minimizes nerve/bone damage)
2. Bone Grafting for Dental Implants
Purpose: Rebuild lost alveolar bone to support implants or prosthetics.
Types:
- Autografts: Patient’s own bone (chin/hip)
- Allografts: Donor bone
- Xenografts: Animal-derived (e.g., bovine)
- Synthetic grafts: Hydroxyapatite, TCP
Procedures:
- Socket preservation (post-extraction grafting)
- Sinus lifts (for upper jaw implants)
- Ridge augmentation (for severe bone loss)
3. Removal of Jaw Cysts & Tumors
Conditions Treated:
- Periapical cysts (from infected teeth)
- Dentigerous cysts (around impacted teeth)
- Odontogenic tumors (e.g., ameloblastoma)
Techniques:
- Enucleation (complete cyst removal)
- Marsupialization (for large cysts, staged removal)
- Resection (for aggressive tumors)
4. Orthodontic Support Procedures
Surgeries to Aid Tooth Movement:
- Exposure of Impacted Teeth (bonding brackets to buried teeth)
- Frenectomy (removing restrictive lip/tongue ties)
- Corticotomy (accelerated orthodontics via bone cuts)
Key Considerations
- Advanced Imaging: CBCT scans for precise planning
- Minimally Invasive Options: Laser or piezoelectric tools for reduced trauma
- Recovery Timeline: Varies by procedure (3-7 days for extractions, months for graft healing)
Chronic Post-Extraction Pain Management Algorithm
A step-by-step guide for diagnosing and managing persistent pain after tooth extraction
1 Initial OMFS Evaluation
- Comprehensive history and clinical examination
- Imaging (IOPA / OPG / CBCT)
If Local Cause Found:
- Retained fragment → surgical removal
- Sequestrum / osteomyelitis → debridement, antibiotics
- Dry socket sequelae → irrigation, curettage
- Oroantral communication → surgical closure ± sinus intervention
- TMJ/muscle pain → physiotherapy, splint, NSAIDs
2 Suspect Neuropathic Pain
- Symptoms: burning, shooting, tingling, hypersensitivity
- Altered sensation on exam (allodynia, paresthesia)
Trial of OMFS-prescribed neuropathic meds:
- Gabapentin / Pregabalin (low dose start)
- Amitriptyline (low dose bedtime)
- Reassess after 2–4 weeks
3 Advanced Medication and/or Neurologist Referral
- Neurological exam + sensory testing
- MRI/MR neurography if needed
Advanced Medical Management:
- Advanced neuromodulators (Gabapentin, Pregabalin, TCAs, SNRIs)
- Carbamazepine / Oxcarbazepine (if trigeminal neuralgia suspected)
- Nerve blocks, botulinum toxin, advanced pain procedures
4 Pain Clinic / Multidisciplinary Care
- Chronic pain specialist
- Psychosocial support / CBT
- Interventional pain management (radiofrequency, cryotherapy, decompression surgery if indicated)
Summary Pathway
Why Choose an Oral Surgeon for Complicated Tooth Extractions?
Expert care for wisdom teeth and complex dental cases in Nepal
Do I need a specialist for my tooth extraction?
When it comes to wisdom teeth removal or other complicated extractions, many patients in Nepal wonder: "Can any dentist do it, or do I need an Oral & Maxillofacial Surgeon?"
General Dentists
Can remove simple teeth with straightforward anatomy
Oral & Maxillofacial Surgeons
Specialize in complicated extractions, especially wisdom teeth with curved roots, teeth close to nerves, or impacted inside the jawbone
When is an Oral Surgeon Needed?
Wisdom Teeth (बुद्धिदाँत) Complications
- Impacted or semi-erupted wisdom teeth
- Deeply curved or hooked roots
- Roots close to the Inferior Alveolar Nerve (IAN) or Sinus cavity
Risk of Nerve or Sinus Damage
- Lower wisdom teeth are very close to the IAN nerve
- Upper molars may be connected to the Maxillary Sinus
- Only an OMFS can safely remove these without long-term damage
Advanced Surgical Techniques
- Bone cutting (osteotomy)
- Tooth sectioning
- Flap design & suturing
- All done with minimal pain and faster healing
Managing Complications Immediately
- If there is excessive bleeding, nerve exposure, oroantral communication, root fracture, or jaw injury, an OMFS can manage it instantly
Better Post-Operative Care
- Pain control, swelling management, antibiotics, and follow-up
- Nerve healing and functional recovery guidance
Benefits of Choosing an Oral & Maxillofacial Surgeon
Safer Results
More predictable outcomes with minimal complications
Faster Recovery
Minimal trauma and quicker healing process
Lower Risk
Reduced chance of nerve injury, sinus issues, or infection
Experienced Hands
Specialized training for complex oral surgeries
Meet Our Specialist
At OraMax Dental Implants & Aesthetics, every surgical case is handled by Dr. Krishna Regmi, Senior Consultant Oral & Maxillofacial Surgeon specialized in:
- Oral Cancer Surgery
- Advanced Dental Implants
- Complex Oral Surgery
Our Locations
OraMax Dental Implants & Aesthetics
Bharatpur, Narayangarh, Chitwan, Nepal
Gaindakot Dental Center
Gaindakot, Nawalpur, Nepal
Dentoalveolar & Minor Oral Surgery
Dr. Krishna Regmi - Oral & Maxillofacial Surgeon
Comprehensive surgical services by Dr. Krishna Regmi, Oral & Maxillofacial Surgeon, including tooth removal, bone and gum surgery, cyst removal, and other procedures essential for oral health and implant preparation.
Procedures & Tentative Rate List
Disclaimer: Rates are tentative and in Nepalese Rupees (NPR). Final cost depends on complexity, anesthesia, imaging, and materials used.
| Procedure | Introduction / Description | Tentative Rate (NPR) |
|---|---|---|
| Tooth Extractions | ||
| Simple Tooth Extraction | Removal of a fully erupted tooth without surgical flap or bone removal. | 3,000 – 6,000 |
| Surgical Extraction | Removal of tooth requiring gum flap or bone removal, often for broken or impacted teeth. | 10,000 – 20,000 |
| Wisdom Tooth Extraction (Partial / Full Impaction) | Specialized extraction for wisdom teeth that are impacted or partially erupted. | 15,000 – 30,000 |
| Surgical Procedures | ||
| Alveoloplasty | Smoothing or reshaping the jawbone after tooth removal to aid healing or denture fitting. | 5,000 |
| Operculectomy | Removal of gum tissue covering a partially erupted tooth, usually wisdom teeth. | 10,000 |
| Incision & Drainage (Intraoral) | Drainage of abscess or infection through the mouth. | 25,000 |
| Incision & Drainage (Extraoral) | Drainage of abscess or infection via skin incision on face/neck. | 40,000 |
| Incisional Biopsy | Removal of a small portion of tissue for diagnosis. | 25,000 |
| Excisional Biopsy | Complete removal of a small lesion or mass for diagnosis and treatment. | 50,000 |
| Enucleation of Cyst | Complete surgical removal of cysts from jawbone or soft tissues. | 80,000 |
| Apicoectomy | Root-end surgery to remove infection when root canal fails. | 20,000 – 35,000 |
| Root Amputation / Hemisection | Removing diseased root of a multi-rooted tooth while preserving healthy portion. | 18,000 – 30,000 |
| Crown-Lengthening | Gum and/or bone reshaping to expose more tooth structure for crown/bridge work. | 18,000 – 35,000 |
| Bone Grafting (Dentoalveolar Area) | Adding graft material to preserve or rebuild bone after extraction or before implant. | 25,000 – 50,000 |
| Tori Removal | Surgical removal of bony growths inside mouth for comfort or dentures. | 20,000 – 40,000 |
| Caldwell-Luc Operation (Root Removal) | Approach through the maxillary sinus to remove displaced tooth root. | 50,000 |
| Caldwell-Luc Operation (Cyst Enucleation) | Removal of large cystic lesions in sinus via surgical approach. | 95,000 |
| Supportive Procedures | ||
| Dressing Charge | Post-surgical wound care and medicated dressing. | 10,000 |
| Suturing (Simple to Multilayer) | Placement of stitches to close wounds, minor to complex. | 15,000 |
| Splinting (Single Tooth) | Stabilizing a loose or injured tooth using wire/composite splints. | 25,500 |
| Splinting (Multiple Teeth) | Stabilization of several mobile teeth. | 28,000 |
| Splinting (Both Arches) | Complete stabilization of teeth in both jaws (additional arch bar charge applies). | 40,000 |
| Intermaxillary Fixation | Wiring jaws together to stabilize fractures or after surgery (screw/arch bar extra). | 40,000 |
| Surgical Excision of Benign Lesion | Removal of non-cancerous growths in the oral cavity. | 70,000 |
| Socket Curettage for Local Osteitis | Cleaning and debridement of infected extraction socket. | 25,500 per site |
| Mucocutaneous Lesion Surgery | Surgical treatment of lesions involving gums, lips, or mucosa. | 30,000 |
| Soft Tissue Laceration Repair | Stitching and repair of cut wounds in mouth or lips. | 40,000 |
What to Expect During Treatment
- Initial evaluation with history, examination, and imaging (X-ray, OPG, CBCT as required).
- Anesthesia: local anesthesia, sedation, or general anesthesia depending on complexity.
- Post-operative care: pain management, diet advice, hygiene instructions, and follow-up visits.
- Additional charges may apply for anesthesia, imaging, grafting materials, or operating theatre use.
Schedule Your Consultation
Contact us for a comprehensive evaluation and personalized treatment plan with exact pricing.
Phone: 9855064961 | Website: www.drkrishnaregmi.com.np
Call Now for AppointmentPost-Extraction Healing Timeline
Day 1-2
Initial healing: mild swelling, slight discomfort. Use cold packs and prescribed painkillers. Avoid rinsing vigorously.
Day 3-4
Swelling peaks then begins to reduce. Eat soft, cool foods. Gentle rinsing can start as advised by Dr. Regmi.
Day 5-7
Discomfort significantly reduces. Normal oral hygiene routines can resume cautiously. Sutures may be removed if used.
Week 2-3
Soft tissue fully heals. Continue regular care and monitor for any signs of infection or complications.
What is Dry Socket?
Alveolar osteitis, commonly called “dry socket,” is a painful condition that can occur after a tooth extraction. It happens when the blood clot at the extraction site becomes dislodged or dissolves prematurely, leaving bone and nerves exposed, causing significant discomfort. Dry socket is most commonly associated with wisdom tooth extractions but can occur after any tooth removal.
Dry Socket Symptoms
Radiating Pain
Pain spreading from the extraction site toward the eye, ear, neck, or temple on the same side of the face.
Visible Bone
Exposure of the underlying bone in the extraction site.
Foul Taste or Smell
Bad breath or unpleasant taste in the mouth due to bacterial activity.
How to Minimize the Risk of Dry Socket
- Follow all post-operative instructions carefully provided by Dr. Krishna Regmi.
- Stop smoking and avoid all tobacco products before and after extraction.
- Discuss any medications with your surgeon, as some may interfere with clotting.
- Avoid vigorous rinsing or brushing near the extraction site for at least 24 hours.
- Avoid using straws for 24–48 hours after extraction to prevent dislodging the clot.
When to Contact Your Surgeon
If you experience severe pain, exposed bone, or a foul taste/smell after extraction, contact Dr. Krishna Regmi immediately. Prompt care helps relieve pain, prevent infection, and ensure proper healing.
Need Help with Tooth Extraction Recovery?
Trust Dr. Krishna Regmi at OraMax Dental & Maxillofacial Surgery for expert care in extractions and post-operative healing.
Call Now: 9855064961Preserving Bone for Dental Implants and Oral Health
The loss or extraction of a tooth can alter the surrounding bone, potentially affecting future dental treatments. Preserving the jawbone after a tooth extraction is integral to successful dental treatment and overall oral health.
Why Preservation is Important
Bone grafting and socket preservation are procedures aimed at maintaining the natural bone structure and contours after tooth extraction or loss. When a tooth is extracted or lost—due to decay or trauma—the supporting jawbone can deteriorate or be resorbed, affecting the stability of adjacent teeth and future treatments such as implants or dentures.
Importance of Natural Teeth
Maintaining bone preserves the structure and density of the jaw. Natural teeth stimulate the bone, while tooth loss can lead to bone resorption over time, affecting future dental procedures.
Support for Adjacent Teeth
Preserving bone prevents adjacent teeth from shifting or tilting into the gap, maintaining proper alignment, a healthy bite, and better outcomes for future restorations.
Preparing for Dental Implants
Dental implants require sufficient bone mass and density. Conserving bone increases the chances of successful implant placement and long-term stability.
Improving Facial Esthetics
Bone grafting and socket preservation maintain natural jaw contours, preventing sunken or aged appearance and ensuring future restorations look natural.
Consult an Oral & Maxillofacial Surgeon
If you are planning a tooth extraction or have lost a tooth, consult with an oral and maxillofacial surgeon (OMS) to discuss bone and socket preservation options. Your OMS will assess your needs and develop a customized treatment plan to meet your oral health goals.
Protect Your Jawbone and Smile
Trust Dr. Krishna Regmi at OraMax Dental & Maxillofacial Surgery for expert care in bone preservation and dental implant planning.
Call Now: 9855064961Dr. Krishna Regmi
Oral & Maxillofacial Surgeon
Tori Removal for Oral Health & Comfort
Expert care to remove benign bone growths and improve oral hygiene, comfort, and denture fit.
Call NowWhat Are Tori?
Tori are benign bone growths inside the mouth, usually on the palate or lower jaw. They are generally harmless but can interfere with eating, speaking, or oral hygiene if large.
Reasons for Tori Removal
- Oral Hygiene: Tori can trap food and plaque, increasing risk of decay and gum disease.
- Discomfort: Large tori may affect eating, speaking, or general comfort.
- Denture Fitting: Tori in denture areas can prevent proper fit and stability.
Assessment & Anesthesia
An oral and maxillofacial surgeon will examine tori size, position, and impact on oral health. Local anesthesia is commonly used, while general anesthesia may be recommended for larger tori.
Procedure
The surgeon carefully removes the tori and reshapes the bone for a smooth, even surface. Sutures may be used and either dissolve or are removed during follow-up.
Recovery & Follow-up
Mild discomfort and swelling are normal and manageable with medications and ice packs. Follow-up appointments ensure proper healing and guidance for oral hygiene and dietary care.
Need Tori Removal?
Consult Dr. Krishna Regmi for personalized evaluation and treatment.
Call NowDr. Krishna Regmi Oral & Maxillofacial Surgeon
Tooth Extraction: Simple vs. Surgical
Expert tooth removal services by Dr. Krishna Regmi. Understanding when simple or surgical extraction is needed for optimal oral health.
Book Your ConsultationUnderstanding Tooth Extraction
Even with proper dental care, teeth age and can decay or break. Many damaged teeth can be repaired with fillings or crowns, but when the damage or decay is excessive, the tooth should be removed. A tooth extraction may not seem complicated, but tooth removal should only be performed by a professional – and in most cases, during a visit to an oral surgeon.
Common Reasons for Tooth Removal
Impacted Wisdom Teeth
Teeth that don't have enough room to emerge properly
Severe Decay
When decay has compromised too much tooth structure
Broken or Fractured Teeth
Teeth with serious cracks extending below the gumline
Crowding Issues
Creating space for orthodontic treatment
Simple vs. Surgical Extraction
Simple Tooth Extraction
Some extractions can be done without making any incisions or using special techniques. This is called a simple extraction, and it may be performed by a general or family dentist or an OMS.
- For visible, fully erupted teeth
- No incisions required
- Performed under local anesthesia
- Quick procedure (10-30 minutes)
- Minimal recovery time
Surgical Tooth Extraction
When a dental professional refers a patient to an OMS for tooth extraction, it is to ensure the tooth is removed or managed with the highest level of expertise.
- For impacted, broken, or severely damaged teeth
- Requires incisions and sometimes bone removal
- May require sedation or general anesthesia
- Longer procedure (30-90 minutes)
- Requires specific post-operative care
The Surgical Extraction Process
The time required to perform a surgical extraction will depend on many factors:
- Position of the tooth
- Length and curvature of the root(s)
- Thickness of bone surrounding the tooth
- The patient's physical health
Assessment & Anesthesia
Comprehensive evaluation and administration of appropriate anesthesia
Incision & Exposure
If gum tissue covers the tooth, an incision is made to expose the tooth
Bone Removal (if needed)
If bone covers part of the tooth, it is removed to fully expose the tooth
Tooth Sectioning
The tooth may be divided into sections for easier removal
Extraction & Cleaning
The tooth is carefully removed and the site is cleaned
Sutures & Aftercare
If an incision was made, sutures are placed to aid healing
After Extraction: The Road to Improved Oral Health
With the exception of wisdom teeth, dental implants are recommended for the replacement of extracted teeth to prevent bone loss and improve functionality. Surgical tooth extraction is simply the first step on the road to improved oral health.
Frequently Asked Questions
Your dentist or oral surgeon will determine the appropriate extraction method based on X-rays and clinical examination. Factors include the tooth's position, condition, and complexity of the roots. Surgical extraction is typically needed for impacted teeth, severely broken teeth, or teeth with complex root systems.
During the procedure, you should not feel pain due to the anesthesia. After the procedure, some discomfort is normal, but it can be managed with prescribed or over-the-counter pain medication. Surgical extractions typically involve more post-operative discomfort than simple extractions.
Initial healing takes about 1-2 weeks, during which you'll need to follow specific aftercare instructions. Complete healing of the bone and soft tissue may take several months. Surgical extractions generally have a longer recovery period than simple extractions.
While generally safe, potential risks include dry socket, infection, nerve injury, or damage to adjacent teeth. These risks are minimized when the procedure is performed by an experienced oral surgeon like Dr. Regmi.
Need a Tooth Extraction?
Schedule a consultation with Dr. Krishna Regmi to determine the best approach for your dental needs.
Call Now: 9855064961